What is De Quervain's disease?
This is a condition which causes pain at the thumb side of the wrist. It is also known as De Quervain's stenosing tenovaginitis and it was first described by a Swiss surgeon in 1895.
Anatomy:
There are many tendons that pass over the back of the wrist joint. These tendons extend the thumb, finger and wrist and they run in separate compartments (tunnels). The compartments are formed by the radius bone and a fibrous sheet of tissue (the extensor retinaculum). These tunnels are lined with synovium which lubricates the tendons enabling them to run smoothly. The first extensor compartment is located over the base of the thumb and it is involved in De Quervain's disease. Two tendons (abductor pollicis longus and extensor pollicis brevis) run through this tunnel.
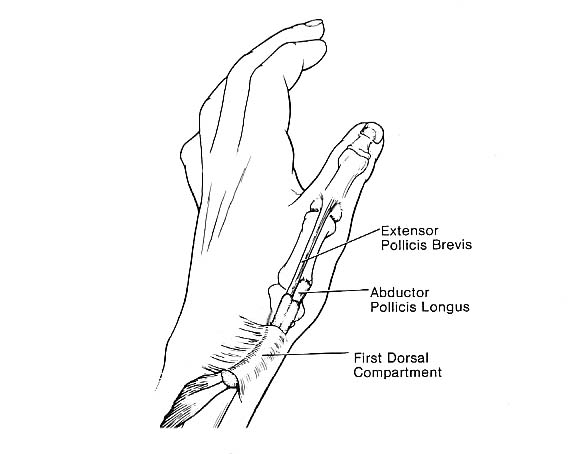 Figure 1: position of the first extensor compartment
Figure 1: position of the first extensor compartment
Causes:
Despite some people referring to the condition as 'tenosynovitis' it is not believed to be an inflammatory condition but due to degenerative changes in the tendon and surrounding tendon sheath. It is therefore more correctly called stenosing tenovaginitis or De Quervain's disease. The end result is thickening and narrowing of the tendon sheath which causes the tendons to catch as they move.
De Quervain's disease is more common in people between 30-50 years old and women are affected more commonly than men. In most cases there is no history of trauma.
Symptoms and signs:
Pain and tenderness over the thumb side of the wrist are typical. This usually develops gradually although in some people it can occur quickly. The pain is typically worse with thumb movements and with activities requiring thumb pinch grip, such as wringing out a cloth or opening jars.
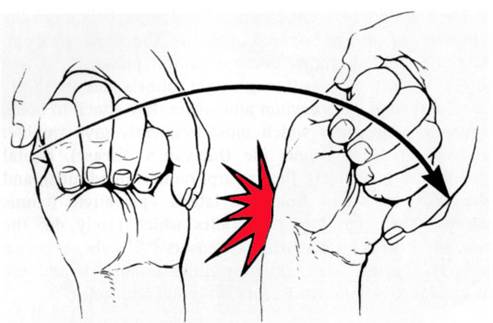
Figure 2: Finkelstein's test. Development of severe pain if the thumb is clasped into the palm of the hand which is then moved towards the little finger
Treatment:
Non-surgical
Many people respond well to non-surgical treatment using the following;
- analgesia medication (especially anti-inflammatory medication, if tolerated)
- use of a splint to rest the wrist and thumb
- physiotherapy
- steroid injection into the first extensor compartment
Surgical
Those patients whose symptoms remain troublesome after non-surgical treatment can consider surgery. The surgery releases the roof of the first extensor compartment to free the tendons. This surgery is performed as a day case procedure using local anaesthesia. Postoperatively many surgeons leave a bulky bandage in place for up to two weeks before it is removed and mobilisation is permitted. In most cases surgery resolves the pain and discomfort.
Surgical complications are uncommon but include
- wound infection (approximately 1%)
- temporary scar tenderness
- numbness or sensitivity over the scar and back of the thumb